A provider’s financial well-being is nearly always tied to the revenue cycle of the clinical practice. The commitment to measuring and monitoring performance is key for making process adjustments and setting appropriate goals. Technology integrated with practice management (PM) systems can accurately automate many RCM processes, which effectively increases cash flow, decreases staffing need, and reduces redundant costs.
Let’s consider 4 key target areas for optimization:
-
-
- Improving coding accuracy from the point-of-care to the claim processing
- Optimizing work distribution based on value and complexity of the encounter/claim
- Recognizing error situations, their root causes and correcting the process
- Recognizing potential fraud situations (intended or unintended)
-
These optimizations are powered by new data innovations: the integration of workflow automation, data automation, artificial intelligence and data analytics – such technological advances have changed business processes in other industries, and now it’s happening to the revenue cycle for the same reasons: it is highly repetitive, driven by complex rules, requires multiple steps, and challenged by manual hand-offs and exceptions. The result: increased revenue capture, lower overhead, improved accounting close.
So how do you go about doing this? It starts with an effective framework. Frameworks describe how to tie different technology platforms into a coherent assembly to serve a business need. As technology keeps expanding into ever more discrete areas of capability, frameworks help us stitch them together to solve a problem.
In this case our framework must integrate the following technological disciplines in the setting of the revenue cycle environment:
-
-
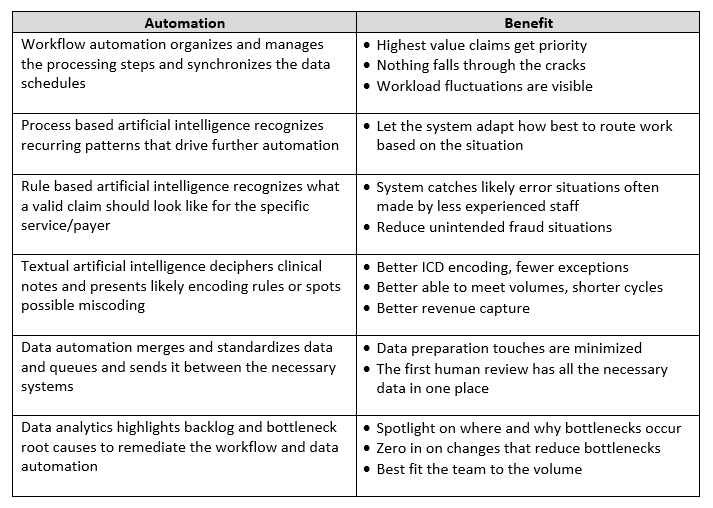
- Workflow automation to organize and manage the processing steps and synchronize the data schedules
- Data automation to merge and standardize data and queues and send it between the necessary systems
- Data analytics to highlight backlog and bottlenecks, root causes to remediate the workflow and data automation
- Process based artificial intelligence to recognize recurring patterns that drive further automation
- Textual artificial intelligence to decipher clinical notes and presents likely encoding rules or spots errors
- Rule based artificial intelligence to recognize what a valid claim should look like for the specific service and prevent unintended fraud
-
Let’s breakdown the benefits of the discrete automation components that are in play here:
Although robust denials management has always been important, it will increase in significance post-ICD-10 as payers and providers wrestle with the nuances of the new code set. In addition, as the industry shifts to value-based care, denials management will become even more essential. As such, workflow management tools are becoming a must-have for organizations looking to remain viable long term.
Finally, before proceeding with any automation solution, you should determine what KPIs that approach can impact and collect a baseline of performance. Regardless of the technology an organization uses, be sure you have a way to analyze whether your investment in a solution has made your targeted areas for improvement.